Retrosternal pain – overview in details
Retrosternal pain is one of the main signs of coronary heart disease (CHD) and myocardial infarction. However, there are several diseases that can cause this symptom. In this article, we will analyze the main causes of chest pain, and also touch a little on the management of patients with this disorder.
Where is retrosternal pain located and what sources can it have?
Retrosternal pain is localized behind the sternum: behind the bone on the anterior chest wall, to which the ribs are attached. All structures of the chest can be its source, namely:
- Heart - angina pectoris, heart attack, pericarditis.
- Other organs of the chest - aortic dissection, irritation of the pleura in pneumonia, pulmonary infarction, pneumothorax, diseases of the esophagus, trachea, bronchi or mediastinum.
- Chest wall - neuralgia, pain in the bones and muscles, diseases of the mammary glands and skin (for example, herpes zoster).
- Abdominal organs - gastroesophageal reflux, pancreatitis.
Psychogenic pain is also singled out separately.
The leading cause of retrosternal pain is an insufficient blood supply to the heart muscle. Three main mechanisms of its occurrence are described below.
- Narrowing of the coronary arteries due to the progression of atherosclerosis.
- Decrease in the supply of oxygen to the tissues of the heart, for example, with a decrease in its concentration in the blood or with anemia.
- Increased oxygen consumption by the heart (often found in hypertrophic cardiomyopathy).
Chest pain can cause many different sensations depending on what is causing the symptom. Often the cause has nothing to do with the heart, but it is almost impossible to determine without visiting a doctor. Below we will analyze the features of pain in various pathologies.
Myocardial infarction and coronary heart disease (CHD)
These two pathologies are inextricably linked with each other. Ischemic heart disease is most common in males. Risk factors for the disease are smoking, obesity, sedentary lifestyle and genetic predisposition.
With CHD, a partial blockage of the vessels of the heart occurs, which provokes insufficient blood flow to the heart muscle and retrosternal pain (angina pectoris). The disease is divided into several degrees depending on the moment of onset of pain. The most severe form is considered to be the one in which the pain syndrome occurs at rest.
With CHD, the pain is of a pressing, compressive nature, can radiate to the arm, lower jaw, in most cases it decreases at rest, and also after taking nitroglycerin.
Myocardial infarction is usually the result of a ruptured atherosclerotic plaque in a coronary vessel that supplies blood to the heart. When the plaque ruptures, a thrombus forms around it, blockage of the coronary vessel occurs and blood flow to the heart is blocked.
With this pathology, the pain lasts more than 30 minutes, is stronger than with angina pectoris, does not weaken at rest or after taking nitroglycerin, and, like with IHD, has a pressing, squeezing character. With this pathology, the doctor often encounters retrosternal pain radiating under the left shoulder blade, into the jaw, abdomen and accompanied by shortness of breath and a feeling of fear of death.
Pericarditis (inflammation of the pericardium, the outer lining of the heart)
This pathology can be caused by pathogenic microorganisms (bacteria, viruses, etc.) or be non-infectious in nature (for example, in autoimmune pathology). With pericarditis, the pain has an acute stabbing character. It can last several hours or days, vary in intensity, give to the neck, left shoulder and shoulder blade, and also increase in the supine position and depend on breathing. The pain syndrome may be preceded by fever, weakness, drowsiness.
Aortic dissection
This disease is a life-threatening pathology and can lead to rupture of the aorta, the largest blood vessel in the human body. With aortic dissection, very severe pain is noted, which is tearing in nature, appears suddenly, can last several hours and radiate to the back and between the shoulder blades. Its localization depends on the location of the dissection (most often behind the sternum and on the anterior chest wall).
Pleural lesion
The pleura is a shell that covers the lungs and has two leaves. Between the latter is the pleural cavity. Pleural pain occurs, for example, with pneumothorax or inflammation, has a stabbing character (less often — baking), increases with deep inhalation or cough, rarely localizes behind the sternum.
Pulmonary embolism (PE)
This disease is a blockage of one of the pulmonary arteries. In most cases, the pathology is triggered by blood clots that enter the lungs from the deep veins of the legs or, less often, from other parts of the body. PE is also a life-threatening condition. Usually, in this condition, pain sensations appear suddenly, resembling those of myocardial infarction. The presence of pain in PE is explained by the expansion of the vessels of the lung root and irritation of the pleura.
Inflammation of the bronchi and trachea
This condition can have both an infectious and non-infectious nature. The pain syndrome is characterized by a baking and dull character, increases with a deep breath, can radiate into the shoulder blade and shoulder, increases with a deep breath.
Da Costa syndrome
This pathology is also called stress syndrome, neurocirculatory asthenia, etc. It has been studied by many outstanding doctors for more than 100 years. It was originally found in men during wartime. However, it was further described in both sexes and peacetime. In this syndrome, the patient complains of chest pain on the left (other localization is less common), chest discomfort, shortness of breath, palpitations, a feeling of suffocation, dizziness.
Although symptoms may appear after infections and various physical and psychological stresses, neurocirculatory asthenia is most often found as a familial disorder. During examination and diagnostic procedures, the doctor usually does not detect deviations from the norms. The origin of this disease remains unclear. Patients have a normal life expectancy. A healthy lifestyle, as a rule, improves the condition of these patients.
What other symptoms can be associated with severe chest pain?
- Shortness of breath. It occurs with pulmonary embolism (PE), cardiogenic pulmonary edema and pneumothorax.
- Cough. It is a frequent symptom of lung abscess (hemoptysis is often observed), pulmonary edema, pulmonary edema together with foamy sputum and pneumothorax (dry cough is usually observed).
- Heartbeat. It is characteristic of atrial fibrillation, PE and pneumonia.
- Increased sweating, nausea and vomiting. Typical for infarction and pulmonary embolism.
What is the algorithm of the doctor's actions in the presence of chest pain in the patient?
First of all, the doctor should rule out life-threatening conditions such as acute coronary syndrome, aortic dissection, aortic stenosis, pericarditis and cardiac tamponade. The doctor should also be aware of threatening conditions from other organs: tense pneumothorax, pulmonary embolism or rupture of the esophagus.
After excluding the above-mentioned acute pathology, the doctor must exclude other diseases and make the correct diagnosis, on which the further management of the patient will depend.
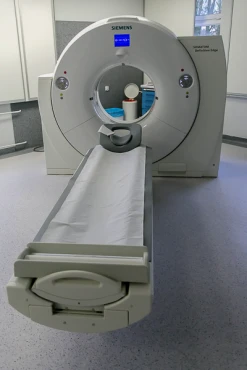
When detecting the disease that caused the chest pain, various diagnostic methods are used, such as radiography, CT, MRI, ECG, laboratory blood tests. In case of suspected pathology of the digestive tract (rupture of the esophagus), an endoscopic examination (FGDS) may be required.
Treatment of patients with pain behind the sternum
As noted earlier, the therapy of this symptom is determined by the cause of its occurrence. Thus, in case of myocardial infarction, most patients need to undergo percutaneous coronary intervention. Esophageal ruptures, aortic dissection are also often treated surgically. With inflammation of the pleura of the pericardium, bronchi and lungs, conservative treatment is used in most cases, for example, antibiotic therapy.
With Da Costa syndrome, the patient needs help from not only a therapist or a general practitioner but also a psychotherapist.
When should I see a doctor?
Chest pain should never be ignored. The doctor's help is especially necessary if a person has not had this symptom before, as well as in the case when a heart attack can be suspected (in the elderly, obese people, etc.). Thus, since chest pain may indicate a serious problem, it is important to seek medical help immediately.
Resume
Chest pain can be a sign of many diseases. The priority for the management of patients with such a symptom is, first of all, the elimination of sources of threat to life. Patients with non-cardiac chest pain may have more than one etiology, and may also have concomitant psychological diseases.
Diagnosis of chest pain can be difficult due to its heterogeneous nature. The classification of this symptom varies in different fields of medicine. For example, gastroenterology uses terminology related to gastroesophageal reflux disease and unrelated to gastroesophageal reflux disease.
Proper diagnosis of chest pain allows you to identify a specific cause, which makes it possible to conduct effective treatment aimed at the underlying disease.
References:
- Cayley W. E., Jr (2005). Diagnosing the cause of chest pain. American family physician, 72(10), 2012–2021.
- Erhardt, L., Herlitz, J., Bossaert, L., Halinen, M., Keltai, M., Koster, R., Marcassa, C., Quinn, T., van Weert, H., & Task Force on the management of chest pain (2002). Taskforce on the management of chest pain. European heart journal, 23(15), 1153–1176.
- Harrison`s Principles of Internal Medicine 19/E (Vol.1). Dennis Kasper, Anthony Fauci, Stephen Hauseret all. McGraw-HillEducation 2015 ISBN: 0071802134 ISBN-13(EAN): 9780071802130.